What is Hepatitis?
The word hepatitis simply means inflammation (titis) of the liver (hepat). Hepatitis can be caused by:
- viruses,
- harmful consumption of alcohol, drugs, medications,
- contact with some chemical and toxins, and
- some autoimmune conditions.
The inflammation in the liver is your body’s natural reaction to the damage being caused by these conditions and toxins.
Hepatitis B and hepatitis C are the most common types of viral hepatitis globally with an estimated 325 million people living with these viruses.
To have a hepatitis D infection you need to have an active hepatitis B infection for the virus to replicate. The transmission route for hepatitis D is also the same as hepatitis B (blood-to-blood contact, sexual contact and mother to child transmission). Hepatitis E is similar to hepatitis A as it is transmitted through faceal-oral route, but they are unrelated.
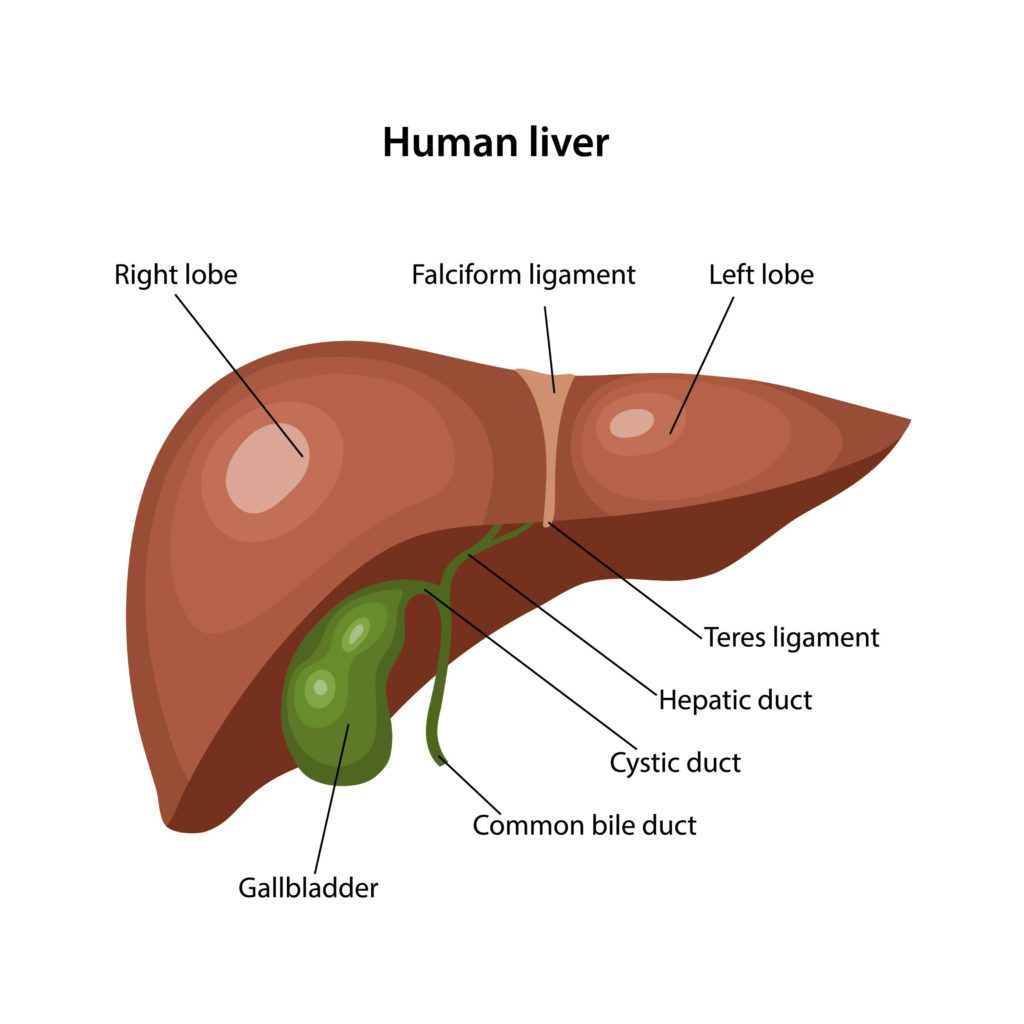
Weighing in at an average of 1.5kgs, the liver is the largest organ inside your body. Your liver is positioned in the top right side of your abdomen, just beneath the diaphragm but above your stomach. The liver is the heavyweight in your body and one of the hardest working organs working “behind the scenes”. It is like a factory, it manufactures, stores, and processes anything that you put in your body, including food, alcohol, medicine, or toxins. It performs over 500 functions!
See Liver Health for more on what your liver does.