Alcohol and hepatitis
Alcohol and hepatitis
How does alcohol affect my hepatitis?
Alcohol is toxic to the liver (hepatotoxic). If you have hepatitis B or hepatitis C, one of the best things you can do for yourself is to cut out drinking or cut down as much as you can.
Alcohol may increase damage to your liver, liver scarring (cirrhosis) and liver cancer (hepatocellular carcinoma). Drinking alcohol can also increase the amount of virus in your body. It’s important that you discuss your alcohol consumption with your doctor or liver specialist.
If you have viral hepatitis, it is best not to drink any alcohol but if you do drink it is important to limit the amount of alcohol to reduce further possible damage to your liver.
How much can I drink?
If you have hepatitis B or C it is recommended that you drink no more than:
- one standard drink per day, WITH AT LEAST
- three alcohol-free days per week.
However, everyone is different. For people with viral hepatitis, alcohol may cause liver or abdominal pains and fatigue the following day so “listen to your liver”! If you have liver scarring or liver cancer, you are advised not to drink any alcohol at all. If you do drink alcohol, monitor your own use and the ways in which alcohol affects you.
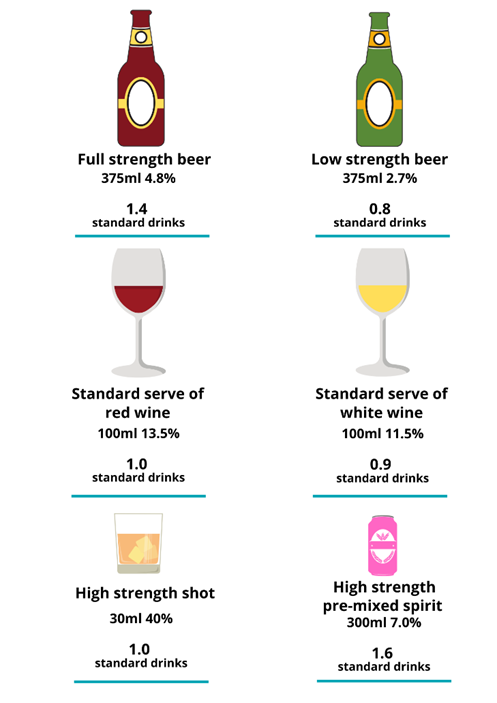
What is a ‘standard drink’?
A standard drink is any drink containing 10 grams of alcohol.
Below is a few different alcoholic drinks showing how many standard drinks they include. For more examples see the Australian Standard drinks guide.
Signs that you might need to cut down on alcohol:
- fatigue
- liver, abdominal or stomach pains
- difficulty managing the amount you drink
- withdrawal symptoms (tremors or anxiety)
- increased stress levels or disrupted sleep
- relationship or sexual difficulties
- increased aggression or violence
- diminished judgement and performance
- remorse
Binge Drinking
Binge drinking occurs when a person drinks heavily over a short period of time resulting in immediate and severe intoxication. Sometimes binge drinking is defined as ‘drinking to get drunk’. Health risks associated with binge drinking include hangovers, headaches, and stomach problems resulting in nausea, shakiness and vomiting.
Can I start hep C treatment if I drink alcohol or use drugs?
Drug or alcohol use is not a restriction with the new direct-acting antiviral treatments. The new guidelines for treatment encourage doctors to treat everyone, even those who drink alcohol and use drugs.
What can I do to help manage my alcohol intake?
If cutting out alcohol entirely is not an option for you, consider reducing the amount you drink, or try one week without any alcohol. Then, note how you felt the week you reduced or gave up alcohol, compared with the week when you drank.
Some simple ways to help you manage your alcohol intake include:
- avoid binge drinking – it places a heavy strain on your liver
- start with a non-alcoholic drink, especially if you are thirsty
- try not to drink in rounds – determine your own drinking pace
- eat a substantial meal before drinking
- alternate alcoholic drinks with non-alcoholic ones
- try new social situations where drinking is not usually expected
- switch to low-alcohol drinks
- have several alcohol-free days per week
Organisations that can help
- Alcohol and Drug Information Service (ADIS) offers confidential and anonymous telephone counselling and information for individuals, parents, and concerned others. ADIS is available 24 hours, 7 days a week by calling 1800 177 833 (free call)
- 13 HEALTH (13 43 25 84) is a confidential phone service that provides health advice to Queenslanders, 24 hours, 7 days a week
- Drinkwise provides general information about alcohol
- Lifeline 13 11 14
Information and Support
If you have a question, call Hepatitis Queensland Infoline on 1800 437 222 or contact us online.