Liver Diseases
Liver disease is a surprisingly common condition affecting many Australians. There are over 100 types of liver disease ranging from mild damage to severe scarring and failure.
On this page you can learn more about:
- Metabolic Associated Fatty Liver Disease (MAFLD)
- Non-Alcoholic Steatohepatitis (NASH)
- Alcohol-Related Liver Disease (ARLD)
- Viral Hepatitis
- Cirrhosis
- Liver Cancer
- Liver Failure
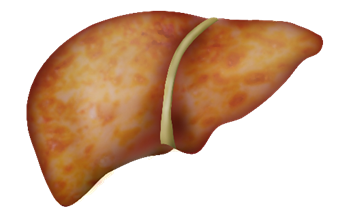
Metabolic associated fatty liver disease or MAFLD is the build-up of fat in the liver. The liver can handle a small amount of fat, but too much will cause inflammation and progress to long-term damage if left untreated.
It is important to note that MAFLD is not caused by alcohol. In the past MAFLD has been referred to as non-alcoholic fatty liver disease (NAFLD).
MAFLD includes a series of liver conditions that people can move through. These include:
- Simple fatty liver (steatosis): Fat begins to develop in the liver
- Non-alcohol related steatohepatitis (NASH): Fat builds up that causes inflammation and damage to the liver
- Fibrosis: Damage has progressed, creating life-long scarring
- Cirrhosis: More severe liver scarring and hardening occurs, putting you at risk of liver failure and liver cancer
MAFLD affects 25% of the Australian population.
What causes MAFLD?
The following increases your risk of developing MAFLD:
- Unhealthy diet
- Overweight or obese
- Type 2 diabetes
- High cholesterol or blood pressure
- Underactive thyroid
- Insulin resistance. E.g. Polycystic Ovary Syndrome (PCOS)
MAFLD symptoms
People living with early stage MAFLD will experience almost no symptoms. If any, you may experience:
- Tiredness
- Discomfort in upper right area of your abdomen (where your liver is)
Treating MAFLD
During early stage MAFLD, treatment will focus on any underlying or associated causes. This may include:
- Healthy dietary changes
- Physical activity and lifestyle changes
- Treatment for other conditions. E.g. diabetes or high cholesterol
- Regular liver health checks
Regular monitoring can help assess whether the damage to your liver is progressing. If your early stage MAFLD has developed into NASH or cirrhosis, other treatment may be advised.
Non-alcoholic steatohepatitis (NASH) is a severe form of fatty liver disease where the liver becomes inflamed (swollen) and scarred (cirrhosis).
It is caused by a build up of too much fat in the liver. Approximately one in 10 people with fatty liver disease will go on to develop NASH.

In the video below liver specialist Dr Graeme MacDonald talks about NASH and fatty liver disease.
What causes NASH?
Not everyone that has MAFLD, or simple fatty liver will develop NASH.
However, those with MAFLD are more likely to develop NASH if they have one or more of the following conditions:
- Obesity
- High blood pressure
- High blood fat levels (triglycerides)
- Abnormal levels of cholesterol
- Type 2 diabetes or insulin resistance
- Metabolic syndrome
NASH symptoms
People living with NASH will often experience little or no symptoms. However, some may experience the following:
- Fatigue
- Loss of appetite
- Abdominal discomfort
- Jaundice (yellowing of the skin and eyes)
- Itchy skin
- Weakness and confusion
If NASH is detected early, you can prevent more damage occurring. If you have any concerns, please talk to your doctor.
Treating NASH
Treatment for NASH is based on managing associated conditions and creating healthy lifestyle changes.
Your doctor may recommend to:
- Lower blood pressure and cholesterol level
- Lose weight
- Reduce or stop alcohol intake
- Regular exercise
- Manage your diabetes
- Regular liver health checks
There is currently no medication to treat NASH but maintaining healthy lifestyle changes will reduce your risk of developing cirrhosis.
What is Alcohol-Related Liver Disease?
Alcohol-related liver disease (ARLD) can occur when you drink too much alcohol. Among other toxins, our liver filters any alcohol we put into our bodies. Drinking too much doesn’t allow the liver enough time to recover causing fat to build up and cause damage.
Alcohol-related liver disease has three stages:
- Fatty Liver (steatosis): Fat builds up in your liver due to harmful alcohol intake, making it harder for the liver to function.
- Alcohol-related hepatitis: The liver becomes inflamed, swollen and tender. This stage can occur either early on or after years of harmful drinking.
- Alcohol-related cirrhosis: Long-term damage to the liver has created permanent scarring and hardening. Your liver function has decreased, and you are at risk of developing liver cancer and liver failure.
About one in 10 people who experience alcohol-related liver disease and continue to drink harmfully will develop cirrhosis.
What causes alcohol-related liver disease?
Excessive alcohol intake is the cause of alcohol-related liver disease, this can be either binge drinking or drinking excessive amounts regularly.
People living with other chronic liver conditions are more at risk of further damaging their liver with alcohol. Even a small amount of alcohol can be harmful, speak to your doctor about what is recommended for you.
Alcohol-related liver disease symptoms
Many people won’t experience any symptoms for alcohol-related liver disease until the condition becomes severe.
If you experience any of the following symptoms, speak to your doctor.
- Fatigue
- Loss of appetite
- Nausea or vomiting
- Discomfort in the abdomen around your liver
- Dizziness
- Jaundice (yellowing of the skin and eyes)
If your alcohol-related liver disease has progressed to cirrhosis, symptoms can include a build up of fluid in the abdomen, confusion or behaviour change, and, kidney or liver failure.
Read more about cirrhosis to understand what to look out for.
Treating alcohol-related liver disease
Reducing or stopping your alcohol intake is the most effective way to lower the chances of your alcohol-related liver disease progressing.
Damage from early stage alcohol-related liver disease can be reversed by reducing or stopping your alcohol intake. Most importantly, all stages of alcohol-related liver disease benefit from cutting out alcohol.
Depending on what stage of alcohol-related liver disease you are experiencing, your doctor can recommend whether any alcohol is safe.
It is also beneficial to maintain a well-balanced, nutritious diet and only take medication approved by your doctor.
Your doctor can recommend support that will help you manage your alcohol intake.
If you are living with cirrhosis, treatment may be different. Read more about cirrhosis treatment.
Hepatitis means inflammation (titis) of the liver (hepat). There are numerous causes of hepatitis, including alcohol-related hepatitis or autoimmune hepatitis, but when we talk about viral hepatitis, we are referring to a blood borne virus that causes inflammation and damage to the liver.
There are a few types of viral hepatitis, however here we are going to focus on the two most common, hepatitis B and hepatitis C.
Read more about the other types of viral hepatitis.
Hepatitis B
Hepatitis B is a blood borne virus that can be spread by blood to blood contact, sexual fluids or from mother to baby during birth. The virus causes inflammation and damage to the liver and can lead to severe liver disease, including cirrhosis and liver cancer.
In 2020, 34,000 people were estimated to be living with hepatitis B in Queensland, many still undiagnosed.
Many people won’t notice the symptoms of hepatitis B until their condition becomes more severe.
Symptoms
You may experience:
- General aches and pains
- Fever
- Nausea
- Loss of appetite
- Abdominal discomfort
- Yellowing of the eyes and skin (jaundice)
- Light coloured faeces and dark urine
Treatment
There is no cure for hepatitis B, but there is a safe and effective vaccine.
If you are living with hepatitis B, it is important to be monitored by a doctor to regularly check your viral load is under control. Some people may need to take medicine to treat their hepatitis B, but others won’t.
The best ways to look after yourself are:
- Have regular six monthly check-ups with your specialist or doctor
- Reduce or avoid alcohol (alcohol can increase your chances of developing cirrhosis or liver cancer)
- Eat a balanced diet
- Get regular exercise
- Reduce your stress and get support
- Try to maintain a healthy body weight
- Rest when you need to.
Without regular monitoring by your doctor, the virus increases your risk of developing more serious liver disease, including liver cancer.
Read more information on hepatitis B transmission, prevention, and treatment.
Hepatitis C
Hepatitis C is a blood borne virus that can be spread by blood to blood contact. The virus causes inflammation and damage to the liver and can lead to serious liver disease, including cirrhosis and liver cancer.
In Queensland, an estimated 43,594 people are living with hepatitis C.
Symptoms
Many people living with hepatitis C will experience little to no symptoms. If you think you might be at risk, it is important to get checked. Read more about hepatitis C testing.
Symptoms some people may experience include:
- General aches and pains
- Yellowing of the eyes and skin (jaundice)
- Nausea
- Abdominal pain and discomfort
- Loss of appetite
- Light coloured faeces and dark urine
- Fatigue and brain fog
Treatment
While there is no vaccine to stop you catching hepatitis C, very successful cures are available. Treatment most commonly involves taking tablets daily for 8 to 12 weeks with little to no side effects.
The medicine will successfully clear the virus for 95% of people, however it is possible to be reinfected if you come into contact with hepatitis C again.
Read more about transmission and prevention to learn about protection against hepatitis C.
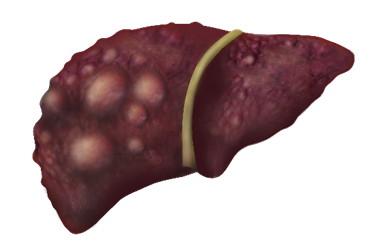
Cirrhosis is the result of long-term, untreated damage to the liver. A liver affected by cirrhosis is full of hard, scarred tissue, which reduces blood flow and liver function.
You may hear about two stages of cirrhosis:
- Compensated cirrhosis means your liver is healthy enough to keep functioning normally, but it has to work a lot harder due to scarring.
- Decompensated cirrhosis means the scarring and hardening of your liver is so severe it can no longer do its job properly.
You will experience different symptoms and require different treatment depending on what stage you are experiencing.

What causes cirrhosis?
Anything that leads to long-term damage of the liver increases your risk of cirrhosis, including:
- Being overweight or obese with a fatty liver
- Fibrosis (mild scarring)
- Harmful alcohol consumption
- Hepatitis B or C
- Some immune system problems
- Inherited or autoimmune liver diseases (such as Haemochromatosis)
Cirrhosis symptoms
People with cirrhosis may experience the following symptoms:
- Tiredness and difficulty sleeping
- Nausea and vomiting
- Poor appetite and weight loss
- Pain in the liver area
- Jaundice (yellowing of the skin and eyes) and itchy skin
- Blotchy red palms
- Spider-like veins on upper body
If you are experiencing severe cirrhosis, you may also experience:
- Vomiting blood and dark stools
- Swelling of the feet, legs, ankles or abdomen
- Shortness of breath
- Fever
- Confusion, drowsiness, or behaviour change
Treating cirrhosis
Treatment depends on the cause and stage of your cirrhosis.
If there is an underlying cause, then it will be managed specific to that cause. For example, a hepatitis C infection will be treated with medication to cure the virus.
In addition to treatment for different liver conditions, you may be advised to:
- Avoid alcohol
- Make healthy diet and lifestyle changes
- Take or avoid certain medications
- Have regular check-ups and liver scans
- Have a liver transplant
Cirrhosis cannot be cured however proper management or treatment can reduce its impact on your health.
Looking after yourself can slow down the build up of scar tissue and prevent more serious conditions such as liver cancer and liver failure.
Talk to your doctor for more information on the right treatment for you.
Liver cancer occurs when abnormal cells grow and multiply to form a mass or lump known as a tumour.
Primary liver cancer is when the cancer starts in the liver. Secondary liver cancer begins elsewhere and travels to the liver. Secondary liver cancer is more common, often spreading from the bowel.
Rates of liver cancer are on the risk with approximately 1 in 103 Australians at risk of being diagnosed with liver cancer by the age of 85. Men are three times as likely to develop liver cancer (1 in 71).
The most common type of primary liver cancer is Hepatocellular Carcinoma (HCC) and begins in our hepatocytes, the key cell of the liver.
Rare liver cancers
Rare liver cancers affect a smaller proportion of the population. These include:
- bile duct cancer
- angiosarcoma
- hepatoblastoma
What causes liver cancer?
Hepatitis B or C viruses are the leading causes of primary liver cancer in Australia. The following conditions also increase your risk of developing Hepatocellular Carcinoma:
- Obesity
- Type 2 diabetes
- Smoking tobacco
- Excessive alcohol consumption
- Family history of liver cancer
Liver cancer symptoms
Someone with liver cancer may experience the following symptoms:
- Tiredness
- Swelling and pain in the stomach
- Pain in the right shoulder
- Nausea, poor appetite, or weight loss
- Jaundice (yellowing of the skin and eyes) or itchy skin
- Fever
- Pale bowel motions
Treating liver cancer
Your doctor may recommend the following treatments:
- Chemotherapy or transarterial chemoembolisation (TACE), a form of chemotherapy directly targeting the tumour
- Liver resection: surgery to remove part of the liver
- Tumour ablation: heat, alcohol injection or freezing that destroys small tumours
- Specialised radiation therapy techniques (SIRT OR SBRT)
- Liver transplant
More information and support
Read more about liver cancer on the Cancer Council website. The Cancer Council also has a range of support services available for patients, family, and friends.
Liver failure is a life-threatening condition and the end stage of many liver diseases.
There are two types of liver failure:
- Chronic liver failure develops slowly, causing a gradual decline in liver function.
- Acute liver failure is a very rare condition, that results in rapid loss of liver function, usually over days to a few weeks.
What causes liver failure?
Chronic liver failure often occurs from cirrhosis, the severe scarring of the liver reduces its capacity to function properly and leads to failure.
Acute liver failure is usually caused by an overdose of a medicine (e.g. paracetamol) or toxin. In some cases acute liver failure is caused by hepatitis, or other liver condition.
Liver failure symptoms
Symptoms of liver failure include:
- Fatigue and feeling generally unwell
- Jaundice (yellowing of the skin and eyes)
- Easy bruising or bleeding
- Swelling around the belly due to fluid building up (ascites)
- Dizziness and confusion
- Vomiting blood or blood in faeces
If you have any concerns, it is important to see a doctor immediately, liver failure is a life-threatening condition.
Treating liver failure
Treatment for liver failure depends on the cause and how quickly the failure is detected. Treatment options include medication and liver transplant.